Overview
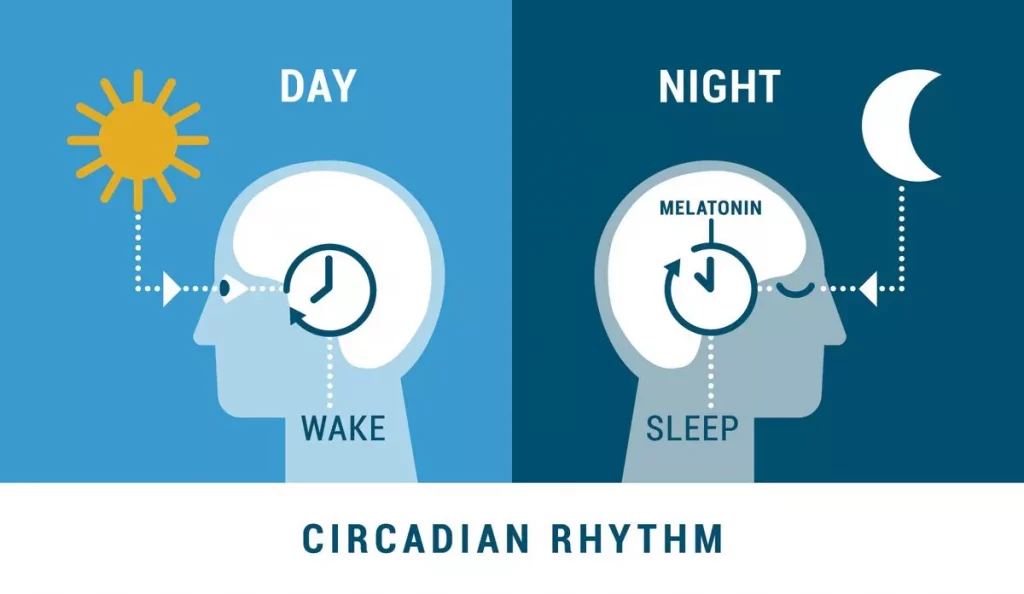
Circadian Rhythm Sleep Wake Disorders refer to a cluster of disorders characterized by abnormal sleeping patterns. Various subtypes in Circadian Rhythm Sleep-Wake Disorders include:
- Delayed Sleep Phase Type: the major sleep period begins at a much later time than conventionally followed (between 2 a.m. and 6 a.m.)
- Advanced Sleep Phase Type: the major sleep period begins at a much earlier time than conventionally followed (between 6 p.m. and 9 a.m.)
- Irregular Sleep-Wake Type: fragmented major sleep period
- Non-24-Hour Sleep-Wake Type: the beginning of major sleep period becomes progressively later every day
- Shift Work Type: trouble sleeping during the day and working during the night in case of individuals on the night shift
Aetiological factors and prevalence usually vary on the basis of subtype, but genetic, biological, neurological, and environmental factors are implicated across the board. Various comorbidities are considered to both, be responsible for the symptoms of the disorder as well as be a product of the same. Various forms of treatment are available, mainly including phototherapy, chronotherapy, behavioral intervention, and melatonin administration.
Signs and Symptoms
The signs and symptoms of Circadian Rhythm Sleep Wake Disorders typically include:
- Sleep disturbances
- Insomnia
- Excessive sleepiness
- Difficulty concentrating
- Low performance at work or school
- Inability to keep up with social commitments
- Trouble with interpersonal relationships and family responsibilities
On the basis of the type of symptoms manifested, Circadian Rhythm Sleep Wake Disorders are classified into the following subtypes:
Delayed Sleep Phase Type
Individuals experiencing Delayed Sleep Phase Type of Circadian Rhythm Sleep Wake Disorders have a pattern of delayed major sleep time in comparison to what is considered conventional. Typically, individuals will find it difficult to initiate sleep before timings between 2 to 6 a.m., and possibly even later.
They also experience difficulties in waking up at desired times in the morning, with excessive sleepiness during the day as well as morning confusion. This delay is usually persistent and lasts for multiple months, and has a variable age of onset, though symptoms may commonly be experienced in adolescence or early adulthood.
Advanced Sleep Phase Type
Contrasting Delayed Sleep Phase Type, this subtype of Circadian Rhythm Sleep Wake Disorders manifests as an unconventionally early commencement of major sleep time, as well as earlier wake times. Individuals may typically sleep between 6 to 9 p.m., and awaken around 2 to 5 a.m.
Excessive daytime sleepiness may be experienced, as well as symptoms of insomnia in the morning time. There is a significant hereditary component associated with Advanced Sleep Phase Type, even though it is considered to be less prevalent in comparison to Delayed Sleep Phase Type.
Usually, the onset of this sleep disturbance may be observed in late adulthood, but it is possible that an earlier onset may be observed in familial forms of Advanced Sleep Phase Type.
Irregular Sleep-Wake Type
Irregular Sleep-Wake Type is a subtype of Circadian Rhythm Sleep Wake Disorders characterized by the absence of a singular major sleep period.
While the total sleep time of individuals with Irregular Sleep-Wake Type is an average amount, it occurs in at least 3 different fragmented sleep sessions distributed throughout the 24-hour day instead of in one continuous sleep period.
The longest sleep session is considered to take place between 2 to 6 a.m., but rarely exceeds 4 hours. Adults with neurodegenerative disorders and children with developmental disabilities commonly present with this subtype of Circadian Rhythm Sleep Wake Disorders. It may also be more common among older adults.
Non-24-Hour Sleep-Wake Type
Individuals with Non-24-Hour Sleep-Wake Type of Circadian Rhythm Sleep Wake Disorders experience a lag between the universally observed 24-hour light-dark cycle and their own internal body clock, or endogenous circadian rhythm.
Owing to this, the commencement of their sleep cycle progressively moves to a later time each day, and can eventually reach a period where individuals sleep during the day and are awake throughout the night. As a result, individuals usually experience insomnia or excessive daytime sleepiness.
This subtype of Circadian Rhythm Sleep Wake Disorders is considered to be more prevalent among individuals with decreased light perception, including blind or visually impaired individuals.
Shift Work Type
Shift Work Type of Circadian Rhythm Sleep Wake Disorders is observable as excessive sleepiness during work and insomnia at home while trying to sleep in the context of regular working hours being outside the daytime window (8 a.m. to 6 p.m.), consisting of workers on the night shift.
Symptoms seem to resolve when individuals return to a daytime schedule, but may be persistent when required to work at night time. While it is known to affect individuals of all ages, those about 50 may be at a higher risk.
Risk Factors
The prevalence and correlates for Circadian Rhythm Sleep Wake Disorders can differ according to the specific subtype in question. The common aetiological factors typically include genetic, environmental, as well as temperamental correlates.
Delayed Sleep Phase Type has been associated with variations in the gene hPER3, which plays a part in determining the length of the overall circadian period. Exposure to light is considered to be an important environmental factor, as does sensitivity to light.
A decrease in exposure or sensitivity to morning light and an increase in exposure or sensitivity to evening light is considered to be linked with this subtype. Brain trauma may also be a correlate, as it may alter the functioning of circadian regulation.
In case of Advanced Sleep Phase Type, a strong hereditary component is implicated, as well as mutations of the PER2 genes, which are also responsible for coding circadian patterns. Environmental patterns such as decreased exposure to light in the late afternoon or early evening as well as exposure to early morning light can advance the circadian rhythm and thus lead to advanced sleep phase.
Behavioral disturbances, such as going to bed early or late can also play a part in causing delayed or advanced sleep phases.
A major correlate of Irregular Sleep-Wake Type is the presence of neurodevelopmental and neurodegenerative diseases. Disorders such as Alzheimer’s. Parkinson’s, and Angelman syndrome can increase the likelihood of irregular sleep-wake patterns.
Neurons in the superchiasmatic nucleus (SCN) are responsible for the regulation of circadian rhythm, and their loss, occurring as an effect of neurodegeneration, is considerably implicated in irregular sleep-wake patterns. Cranial tumours that may affect the SCN may also increase the likelihood of the development of Irregular Sleep-Wake Type of Circadian Rhythm Sleep Wake Disorders.
Non-24-Hour Sleep-Wake Type is largely associated with visual impairment and decreased light perception, but also occurs among those with normal vision.
A lack of light input to the SCN is implicated as being correlational to the discordance between 24-hour cycles and internal circadian rhythms.
A decreased sensitivity to this light in spite of normal perception of it is largely speculated as being associated with the occurrence of this subtype in individuals with functioning sight. Non-24-Hour Sleep-Wake Type is largely comorbid with mood disorders including bipolar and depressive disorders.
The main determinant of Shift Work Type of Circadian Rhythm Sleep Wake Disorders is a requirement to work during usual sleep times, as is practice during night shifts. However, it is possible that some individuals develop Shift Work Type and others do not in spite of being in the same conditions.
While the reasons for the same remain largely unclear, individual differences determined by biological genetic and neurological factors are speculated to have some impact. Individuals with the disorder may have shorter durations of sleep and may also require shorter amounts of time to fall asleep.
Increased sensitivity to new stimuli and decreased sensitivity to auditory stimuli may also be observed among those with a higher likelihood of developing the disorder. Individuals with Shift Work Type may have to deal with difficulties in personal and social lives, with odd working times burdening their interpersonal relationships.
Due to great functional consequences, the risk of development of comorbid disorders such as alcohol use disorder, substance use disorder, and depression may be heightened. Problems such as obesity, cardiologic disorders, gastrointestinal disorders and reproductive health issues may arise.
Diagnosis
A thorough case history is a vital part of determining a diagnosis of Circadian Rhythm Sleep Wake Disorders, as the individual’s account of their sleeping habits is necessary in order to conclude a specific subtype. Additionally, in most cases, a wrist actigraphy may be carried out.
Actigraphy allows the monitoring of activity and rest periods through motor activity. A sleep diary may also be used in order to get an account of sleeping patterns. The duration for which a sleeping diary must be kept differs according to suspected subtype, but typically must be kept for between 7 to 14 days.
Certain assessments and questionnaires may also be used to support a diagnosis. Dim light melatonin onset (DLMO) refers to the body’s natural tendency to start producing melatonin in dim lights two hours prior to sleep time.
The measurement of DLMO can help to objectively determine an individual’s circadian phase. Further, the morningness-eveningness questionnaire (MEQ) can give a better idea of an individual’s preferences of activity and rest, indicating whether they prefer to be more active during the morning or the evening.
The DSM-5 provides the following criteria for the diagnosis of Circadian Rhythm Sleep Wake Disorders:
- A persistent or recurrent pattern of sleep disruption that is primarily due to an alteration of the circadian system or to a misalignment between the endogenous circadian rhythm and the sleep-wake schedule required by an individual’s physical environment or social or professional schedule.
- The sleep disruption leads to excessive sleepiness or insomnia, or both.
- The sleep disturbance causes clinically significant distress or impairment in social, occupational, and other important areas of functioning.
Specify whether:
- Delayed sleep phase type: A pattern of delayed sleep onset and awakening times, with an inability to fall asleep and awaken at a desired or conventionally acceptable earlier time.
Specify if:
- Familial: A family history of delayed sleep phase is present.
- Overlapping with non-24-hour sleep-wake type: Delayed sleep phase type may overlap with another circadian rhythm sleep-wake disorder, non-24-hour sleep-wake type.
- Advanced sleep phase type: A pattern of advanced sleep onset and awakening times, with an inability to remain awake or asleep until the desired or conventionally acceptable later sleep or wake times.
Specify if:
- Familial: A family history of advanced sleep phase is present.
- Irregular sleep-wake type: A temporally disorganized sleep-wake pattern, such that the timing of sleep and wake periods is variable throughout the 24-hour period.
- Non-24-hour sleep-wake type: A pattern of sleep-wake cycles that is not synchronized to the 24-hour environment, with a consistent daily drift (usually to later and later times) of sleep onset and wake times.
- Shift work type: Insomnia during the major sleep period and/or excessive sleepiness (including inadvertent sleep) during the major awake period associated with a shift work schedule (i.e., requiring unconventional work hours).
- Unspecified type
Treatment
While the implications of the different subtypes of Circadian Rhythm Sleep Wake Disorders vary, treatment modalities typically include means such as light therapy, administration of melatonin, or the avoidance of light exposure at certain times.
Chronotherapy is a method through which an individual progressively changes their time of sleep by a few hours until the desired time is achieved, and may be used in delayed or advanced sleep phase types.
Light therapy or phototherapy utilizes bright light to achieve results, and is administered for treatment of disorders other than sleep disorders as well, such as Seasonal Affective Disorder.
Exposure to bright light upon waking or in the last two hours of the sleeping period may advance the circadian phase, and bright light during the evening can delay the circadian phase.
On the basis of the specific subtype experienced, the administration of bright light may be changed by the clinician. The intensity of the light is also of importance. Higher intensity may be preferable in the morning while a lower intensity may be used at night. White lights are usually suggested.
Behavioral interventions are also considered to have efficacy in the treatment of Circadian Rhythm Sleep Wake Disorders. Creating activity schedules and timing sleep periods may be carried out.
Cognitive Behavioral Therapy methods may be used in order to deal with insomnia. Cognitive restructuring and relaxation techniques may be focused on, as well as sleep restriction and hygiene. Controlling the environment where one is sleeping may be recommended on the basis of existing conditions.
Differential Diagnosis
1. Normative variations in sleep: Delayed sleep phase type must be differentiated from late sleep schedule that does not cause personal, social, or occupational distress which is usually seen in adolescents and young adults.
2. Other sleep disorders: Excessive sleepiness may also be caused byother sleep disturbances, such as breathing-related sleep disorders, insomnia, sleep related movement disorders, and medical, neurological, and mental disorders.
Comorbidity
Delayed sleep phase type is associated with depression, personality disorder, and somatic symptom disorder or illness anxiety disorder along with sleep disorders, such as insomnia disorder, restless legs syndrome, and sleep apnea, as well as depressive and bipolar disorders and anxiety disorders.
Delayed sleep phase type may overlap with another circadian rhythm sleep-wake disorder named non-24-hour sleep-wake type. Individuals with non- 24-hour sleep-wake type disorder commonly also have a history of delayed circadian sleep phase.
Specialist
Individuals may approach general practitioners or primary healthcare providers with complaints of insomnia or excessive daytime sleepiness. Physicians may refer patients to sleep specialists, psychiatrists, or clinical psychologists on the basis of an initial assessment and history.
In certain cases, neurologists may also be considered. On the basis of treatment modality, appropriate specialists and therapeutic practitioners may be involved.